Understanding the Different Types of PCOS: A Comprehensive Guide
Navigating the overwhelming amount of information surrounding Polycystic Ovary Syndrome (PCOS) can be stressful, especially after receiving a diagnosis and turning to Google and social media for answers.
Like many of you, when I received my PCOS diagnosis, I found myself scrolling the internet in search of clarity and insights.
However, instead of finding answers, I encountered a sea of conflicting information that only added to my confusion.
During my searches for answers, I first encountered posts on, "What's your PCOS type?"
This introduced me to categorising PCOS into different types, a previously unfamiliar concept and quite frankly excited me. Aha is this the missing piece my doctor didn’t tell me about?
It wasn’t until my university days that I decided to dig deeper into PCOS types such as Insulin Resistant PCOS, Adrenal PCOS, Inflammatory PCOS, and Post Pill PCOS.
While these classifications are widely discussed in many PCOS books and the digital world, unfortunately, they often lack any research-based evidence behind them.
In this blog post, we will explore these four types of PCOS, what scientific research says about PCOS types and what this may mean for you.
So let's dive in.
What is PCOS?
Polycystic Ovary Syndrome (PCOS) is a complex endocrine disorder affecting women of reproductive age worldwide.
It is characterized by a combination of signs and symptoms that include irregular menstrual cycles, high levels of androgens, and polycystic ovaries visible through ultrasound.
What causes PCOS is not completely understood, but it is believed to involve a combination of genetic, hormonal, and environmental factors.
Affecting approximately 1 in 10 women of childbearing age, PCOS is one of the most common hormonal disorders.
Its impact on women's health is profound, extending beyond fertility issues to include increased risks of diabetes, obesity, metabolic syndrome, and cardiovascular diseases.
The condition also significantly affects a woman's mental health, with higher instances of depression, anxiety, and body image issues reported among women with PCOS.
Signs and Symptoms of PCOS
Signs and symptoms of Polycystic Ovary Syndrome (PCOS) can vary significantly from one person to another. Common signs and symptoms include:
Irregular periods or no periods: Periods may be irregular or even absent.
Oligo-anovulation: reduced ovulation, impacting fertility
Infertility: Difficulty getting pregnant.
Hirsutism: excess body hair on the face and body.
Alopecia: Hair loss.
Acne: Skin breakouts.
Skin tags: Small, often harmless growths on the skin.
Weight Gain:Putting on weight, especially around the waist
The diagnostic Criteria for PCOS
The criteria for diagnosing Polycystic Ovary Syndrome (PCOS) have evolved significantly over the years, reflecting its complex nature.
The most widely accepted diagnostic criteria today is the Rotterdam criteria, you can read more about the history of the diagnostic criteria here.
In 2012 the NIH Consensus affirmed the use of the 2003 Rotterdam criteria but also made specific references to include specific Phenotypes.
The Rotterdam criteria suggest diagnosing PCOS if any two of the following three criteria are present:
Clinical or biochemical hyperandrogenism
Oligo/Anovulation
PCOM, with the exclusion of other relevant disorders.
Before we dive into what are the phenotypes let's dive into the 4 PCOS types that you may have come across online, Insulin Resistant PCOS, Adrenal PCOS, Inflammatory PCOS, and Post Pill PCOS.
What are the 4 types of PCOS according to social media?
In recent years, online forums, health blogs, and social media have seen discussions about the four types of PCOS, each with specific treatment recommendations.
These classifications are not formally recognised in research or used in clinical settings. The four PCOS types include Insulin Resistance PCOS, Adrenal PCOS, Inflammatory PCOS, and Post Pill PCOS.
Insulin Resistance PCOS
Anywhere up to 85% of women with PCOS have Insulin resistance.
Insulin resistance develops when the body's cells become resistant to insulin and require higher insulin levels to maintain normal blood glucose levels.
Symptoms often include weight gain, fatigue, excess hair growth (hirsutism), and irregular menstrual cycles. Insulin resistance can be caused by genetic and lifestyle factors and treatment options focus on improving insulin sensitivity.
The concept of "insulin resistance PCOS" is said to be the most common type of PCOS but lacks support from scientific research. While insulin resistance is a common feature of PCOS, it's not accurate to categorise PCOS solely based on insulin resistance.
Adrenal PCOS
Adrenal PCOS is said to be caused by stress and inflammation that produces an excess production of androgens from the adrenal glands, rather than the ovaries.
Symptoms may include severe acne, male pattern hair loss, excess hair growth and irregular periods.
While adrenal androgen excess can contribute to PCOS symptoms, it's not accurate to classify PCOS solely based on adrenal gland dysfunction.
Inflammatory PCOS
Inflammatory PCOS is said to be caused by chronic low-grade inflammation in the body.
Signs of inflammation can present as symptoms such as weight gain, irregular periods, acne, and skin issues.
Chronic inflammation is associated with various aspects of PCOS, including insulin resistance and androgen production, contributing to the complexity of the syndrome.
However, categorizing PCOS solely based on inflammation is challenging due to the heterogeneous nature of the condition.
Post Pill PCOS
Post-pill PCOS, also known as pill-induced PCOS, is described as a temporary condition that can emerge after stopping the use of hormonal contraceptives.
The theory suggests that the oral contraceptive pill may mask underlying hormonal imbalances, which become apparent once pill use is discontinued, mimicking PCOS symptoms.
While some individuals may experience irregularities in their menstrual cycles after discontinuing birth control pills, attributing these symptoms solely to "post-pill PCOS" lacks support from scientific research.
Four PCOS Phenotypes According To Research
In 2012, the NIH confirmed the Rotterdam criteria diagnosis and also made a specific reference to include specific phenotypes.
The creation of phenotypes for PCOS was an attempt to refine the diagnostic process to better capture the diverse presentations of the syndrome and to help healthcare providers with treatment recommendations.
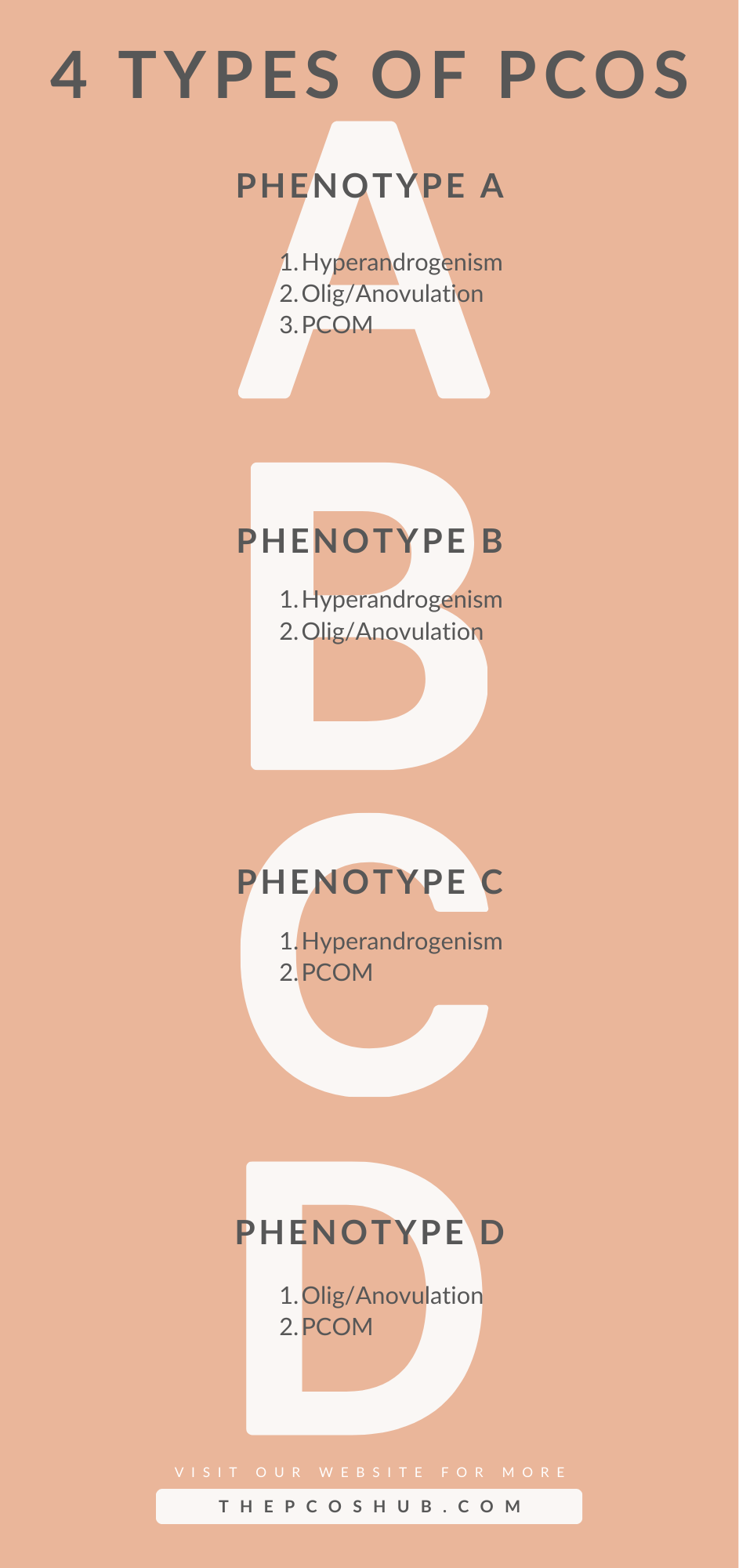
The four PCOS phenotypes:
Type A: delayed ovulation, hyperandrogenic, and polycystic ovaries on ultrasound.
Type B: delayed ovulation, hyperandrogenic, with normal ovaries on ultrasound.
Type C: Hyperandrogenic, with polycystic ovaries on ultrasound and regular ovulation.
Type D: Delayed ovulation, with polycystic on ultrasound and without androgenetic signs.
Phenotype A: known as classic PCOS
Hyperandrogenism: High androgens/androgenic signs
Olig/Anovulation: Irregular periods/delayed ovulation
PCOM: Polycystic ovaries
Phenotype B: classic PCOS
Hyperandrogenism: High androgens/androgenic signs
Olig/Anovulation: Irregular periods/delayed ovulation
Normal ovaries
According to data from clinical populations, women diagnosed with phenotypes A and B are more likely than those with phenotypes C and D to have more severe menstrual dysfunction, higher rates of insulin resistance, a higher risk of metabolic syndrome, and a higher prevalence of obesity.
Phenotype C: non-classic PCOS
Hyperandrogenism: High androgens/ androgenic signs
Regular periods
PCOM: Polycystic ovaries
In comparison to individuals with "classic" PCOS phenotypes A and B, people with phenotype C PCOS typically exhibit intermediate levels of serum androgens, insulin, atherogenic lipids, hirsutism scores, and prevalence of metabolic syndrome.
Phenotype D: non-classic PCOS
Normal androgens
Olig/Anovulation: Irregular periods/delayed ovulation
PCOM: Polycystic ovaries
D-phenotype Patients with this phenotype often had the lowest rate of metabolic syndrome and the mildest endocrine and metabolic conditions in most investigations.
In comparison to participants with classic PCOS, these women had lower levels of total and free T levels, lower LH to FSH ratios, and higher levels of sex hormone-binding globulin.
Distribution of Phenotypes in PCOS According to published data, phenotype A is exhibited by over half of women with PCOS found in a clinical setting.
All things considered, it appears that the classic form of PCOS (phenotypes A and B) accounts for approximately two-thirds of all PCOS cases.
Management of PCOS Phenotypes
Management of your PCOS involves managing the specific symptoms you are experiencing while paying attention to and reducing potential future health problems.
From a dietary intervention perspective, we are not at that level yet in terms of not being able to make targeted suggestions of for example what phenotype A should do as opposed to what phenotype B should do.
While the understanding of PCOS phenotypes is still evolving, healthcare providers can work closely with you to address your unique symptoms, needs and goals.
Even though we may not yet have targeted dietary interventions for each phenotype, there is lots of research showing lifestyle interventions can lead to positive health outcomes for women with PCOS.
Small changes in diet, exercise, and lifestyle habits can have significant benefits in managing PCOS symptoms and reducing future health problems.
Lifestyle Tips for PCOS Management
Living a healthy lifestyle is crucial for managing PCOS effectively. By making lifestyle changes and mindful choices in your diet, exercise routine, stress management, and sleep habits, you can positively impact your overall well-being and alleviate PCOS symptoms.
Diet
A balanced diet is essential for those who have PCOS. The ideal diet for PCOS does not exist.
Try to consume 30–40% of your total calories from carbohydrates in moderate amounts. Make sure the majority of your carbohydrates are from low-GL sources. Raise your protein consumption to 20–30% of your whole diet and concentrate on including roughly 30% of unsaturated fats in your diet.
To support your PCOS, opt for whole foods, lean proteins, fruits, and vegetables to support your PCOS.
Exercise
Regular physical activity plays a significant role in managing PCOS. Engage in a combination of cardio and strength training exercises to support hormone regulation and weight management.
Find an activity you love to do so that you are more likely to be consistent with it.
Aim for at least 150 minutes of moderate-intensity exercise per week. That’s a total of 2 hours and 30 minutes. You could do 30 minutes of exercise across 5 days.
Stress
Chronic stress can exacerbate PCOS symptoms. Incorporate stress-reducing activities into your daily routine, such as mindfulness meditation, spending time with friends and family, deep breathing exercises, yoga, or time in nature.
Prioritising self-care and relaxation to help manage stress levels is important in PCOS.
Sleep
Quality sleep is essential for hormone regulation and overall health, especially for individuals with PCOS.
Aim for 7-9 hours of restful sleep each night. Create a relaxing bedtime routine, limit screen time before bed, and ensure your sleep environment is conducive to quality rest to support your well-being.
Incorporating these lifestyle tips into your daily routine can empower you to better manage PCOS and improve your quality of life. Remember, small changes can lead to significant improvements in your PCOS.
That's all for now; I hope this post helped you to understand the different PCOS types you see online and the phenotypes that are recognised in the diagnostic criteria.
Remember that with PCOS, there is currently no specific diet that is recommended for each phenotype but with the right approach, you can effectively manage your symptoms and improve your overall health.
The good news is that you can determine which dietary and lifestyle modifications are best for you with the help of a registered nutritionist.
This is where my one-on-one program can help you. We can determine the best nutrition and lifestyle through individualised sessions, and we'll put together a customised plan that meets your specific requirements.
With a customised plan of action, we can work together to improve managing your PCOS symptoms. Stay tuned!
Keep an eye out for future posts where we dive deeper into specific aspects of PCOS management.
Together, we can navigate the complexities of PCOS and lead happier, healthier lives.
And remember share this valuable information with your loved ones who might also find this knowledge about PCOS helpful.
As always,
Keep learning, and growing, and stand strong!